Skin Cancer
Cancer of the skin is the most common of all cancers. Millions of cases of skin cancer occur in the world each year including an increasing number in the people of the Middle East. Skin cancer most often occurs among older, fair-skinned people. Most skin cancers are either the basal cell or squamous cell type. These types of cancer tend to grow slowly and spread little and most of them can be cured.
Malignant melanoma is a much more serious form of skin cancer. It was once rare but its rate is now increasing faster than any other type of cancer- 4% every year. The lifetime risk of developing melanoma is now about one in 70 people and this is expected to rise.
The Functions and Structure of the Skin
A group of body tissues with special functions, the skin is actually the largest organ of the body. As a covering or barrier, the skin protects structures underneath from injury, blocks the entrance of bacteria, and prevents the loss of too much water or other fluids. The skin also regulates body temperature, helps rid the body of excess water and salts, and serves as a sense organ for touch, pressure, cold, heat, and pain. In performing its functions, the skin is helped by the hair, nerves, and glands within it.
The skin has three main layers. The lower level is the subcutaneous fat. The middle level of connective tissue is the dermis. The thinnest, uppermost level is the epidermis.
Cancer is really a number of diseases caused by the abnormal growth of cells. Normally the cells that make up the body divide and reproduce in an orderly manner, so that we can grow, replace worn-out body tissue, and repair injuries. Sometimes, however, cells get out of control, divide more than they should, and form masses known as tumors.
Some tumors may interfere with body functions and need to be removed, but do not spread to other parts of the body. Generally, these are known as benign tumors. Malignant, or cancerous, tumors not only invade or destroy normal body tissue, but, by a process known as metastasis, cells can break away from the original tumor and go to other parts of the body. There they may form additional malignant tumors.
Although basal and squamous cell cancers do not usually spread to other parts of the body, they can do so, and are therefore considered malignant. Melanoma is much more likely to spread to other organs, particularly the lungs, liver, and bones.
Types of skin Cancer
There are more than three different types of skin cancer, but the three listed here account for the majority of malignant skin tumors. Other malignant skin conditions can be caused by cancers of the lymph system, of the glands within the skin, and by Kaposi's sarcoma, a connective tissue cancer that sometimes develops in patients with AIDS.
Basal Cell Carcinoma. About 75% of all skin cancers are the basal cell type. They develop in the layer of cells that forms the base of the epidermis, usually on the face, trunk and ears. Once thought of as a disease of middle or older age, basal cell cancer is being seen more and more often among younger people. This rise among younger people is believed to be primarily due to suntanning.
Basal cell cancer is slow growing and does not usually spread to distant parts of the body. If neglected, however, basal cell cancer can spread to nearby areas and invade the bone and other tissues beneath the skin.
A person who develops basal cell cancer is at risk of having the cancer recur in the same place or of developing a new basal cell cancer elsewhere. Within five years, 35% of patients diagnosed with one basal cell cancer will develop a second basal cell carcinoma.
Squamous Cell Carcinoma. Accounting for about 20% of all skin cancers, squamous cell cancers also arise from the epidermis. They most commonly appear on sun-exposed areas of the body such as the face, ear, neck, lip, and hand. They can also develop within other skin lesions like scars or ulcers.
Squamous cell cancers tend to be more aggressive than basal cell cancers and are more likely to invade structures beneath the skin or lymph nodes. They are also more likely to spread to distant parts of the body. Still, only about 3% do so, although this figure rises to about 20% for squamous cell cancers that form in burn or x-ray scars.
Melanoma. Less common, but more dangerous than either basal cell or squamous cell cancers, melanoma begins in cells known as melanocytes. These cells produce the coloring or pigment known as melanin. When exposed to sunlight, the melanin in normal melanocytes turns darker to produce a tan that can help protect the body from burning. Because malignant melanoma cells still produce the pigment, these tumors often include shades of brown and black.
Among white men, melanoma most frequently appears on the trunk; among white women, on the lower leg. The palms, skin under the nails, and the soles of the feet are the most common areas for melanoma to develop among blacks. Melanoma is much more likely than the other forms of skin cancer to metastasize or spread to other parts of the body Melanoma is curable when diagnosed early, hence the importance of screening and early detection. Melanoma that spreads only to nearby areas, usually the lymph nodes, can be cured in any cases. Although some cases of melanoma that have spread to distant parts of the body can be cured, most cannot. That is why melanoma accounts for only 5% of the skin cancer cases, but 75% of the deaths.
 |
 |
| Basal cell Carcinoma of the left upper lip coexisting with Squamous cell carcinoma of the mid lip |
Malignant melanoma |
Precancerous Skin Conditions
Solar keratoses, or actinic Keratoses, are flat, scaly, reddish patches caused by overexposure to the sun. They usually develop on the head, shoulders, and hands of middle-aged people. Actinic keratoses are slow-growing and most often cause no symptoms or signs other than the visible patches on the skin. It is possible, but not common, for solar keratoses to turn into squamous cell cancer.
Even though most Actinic keratoses do not become cancers, they are a warning that a person's skin has become damaged by the sun and that regular self-inspection of the skin and examinations by a doctor are needed. Most actinic keratoses and other skin conditions which could become cancers should be removed. This is traditionally done using liquid nitrogen or preferably laser resurfacing, which heals faster and better. However, more recently research done by Dr. Touma has shown that photodynamic therapy is ideal for the treatment of diffuse actinic damage and actinic keratoses of the face.
Skin Cancer Risk Factors
The main cause of skin cancer is overexposure to sunlight. Fair-skinned people, especially those with red or blond hair, are most likely to get skin cancer. This is because their skin cells have less melanin, the pigment that helps prevent burning. The darker the skin, the more melanin present. Blacks, who have the greatest amount of melanin, are the least likely to develop skin cancer, and if it does occur, it is almost always in skin with less pigment, such as the palms and soles.
People who work outdoors, such as farmers and construction workers, and those who go boating often, play a lot of outdoor sports, sunbathe on the beach or use tanning parlors(solarium) regulary, are at the highest risk of developing skin cancer.
The average age for the discovery of a first non-melanoma skin cancer is about 50. It rarely occurs in childhood, although skin cancer is becoming more common among younger people. Melanoma may develop anywhere from the midteens and onward. Children or teenagers who suffer severe, blistering sunburns are more likely to later develop melanoma.
The sun's rays are the strongest from 10 a.m. to 3 p.m., and whenever possible, exposure to the sun should be avoided during those times. Those who are exposed to the sun should use a sunscreen lotion with a sun protection factor (SPF) of 15 or more, and wear enough clothing to cover the skin as much as possible and wide brimmed hats. Sunscreens should be used even when swimming, since the sun's rays can reach down one meter into the water. Parents should remember to take these steps to protect their children from too much exposure to the sun.
Certain moles make it more likely that a person will develop melanoma. One type of mole, the dysplastic nevus, has varying shades of brown, black, and pink within a single mole, and irregular or uneven borders, with the coloring fading into the skin around the mole. Dysplastic nevi can appear on areas that are often exposed to the sun, and areas that are usually not, such as the buttocks and scalp. They are often larger than other moles. Some people have many such moles, but just one is enough to increase the risk of melanoma.
Dysplastic nevi are often common to members of the same family; 50% of those who have family members with the moles are likely to develop them themselves. Those who have one or more dysplastic nevi and two or more close relatives with malignant melanoma, have a 50% or greater risk of developing melanoma themselves.
Although dysplastic nevi tend to run in families, the moles are not usually present at birth. Rather, they begin to appear in older children and teenagers. In families with a history of melanoma, skin examinations to look for dysplastic nevi should begin when children are age 8 to 10. If none are found then, the child should have another examination at age 12 to 14.
Another type of mole linked to melanoma is present at birth. This is the congenital melanocytic nevus, often called a birthmark. The risk of developing melanoma, as well as basal and squamous cancers, is also increased for those with some rare, inherited conditions that usually start in childhood such as Xeroderma pigumentosa. Ionizing radiation, the type given off by x-rays, can increase the risk of skin cancer for those who often use x-rays in their work, such as dentists and radiologists, and for those who have received x-ray treatments for acne and other conditions. Other less common risk factors include long-term contact with coal tar, arsenic, and other industrial compounds. Arsenic may still be present in some well water.
Looking for signs and symptoms of skin cancer
Any unusual sore, lump, blemish, other skin marking, or change in the way an area of the skin looks or feels may be a sign of skin cancer or a warning that it is likely to occur. The skin might be crusty, scaly, oozing, or bleeding. In later stages of the disease, the skin may also feel itchy, tender, and painful. Most skin problems do not turn out to be cancer, but only tests done by a dermatologist can tell for sure whether a growth on the skin is a cancer or might lead to cancer.
Only those who already know what their skin normally looks and feels like and are familiar with its pattern of moles, blemishes, freckles, and other marks will be able to note any changes in the skin. The best way to become familiar with your normal skin is to examine it regularly, about every 6 to 8 weeks. The best time to do this is after a bath or shower, standing in front of a full-length mirror. A hand-held mirror can be used for those areas that are hard to see. The palms and soles, the spaces between the fingers and toes, and the scalp should also be examined.
Basal cell cancers often first appear as small round or oval patches, shiny and firm, usually white or gray, but sometimes pink or red papules, squamous cell cancers appear more inflamantory are usually small, round, slightly raised, and red and crusty. Often there is a sore in the center that does not heal.
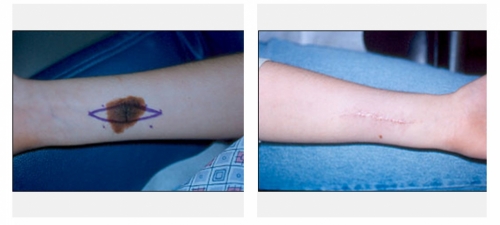
Although melanomas can appear on any area of the skin, they often occur within a mole. That is why it is important to become familiar with moles and note any changes. The ABCD rule can be used to help tell a normal mole or other marking from one that could be melanoma.
ABCD stands for:
Asymmetry - One half does not match the other.
Border Irregularity - The edges of the mole are ragged, notched, or blurred.
Color - The color is not the same over all of the mole, but may be differing shades of tan, brown, or black, sometimes with patches of red, white, or blue.
Diameter - The mole is wider than 6 millimeters (1/4") or is growing larger.
 |
 |
| Atypical nevus. Note large size, irregular border and color | Patient with multiple atypical nevi |
How the diagnosis is made
The diagnosis of skin cancer begins with a complete medical history and inquiry about family history of skin cancer, dysplastic nevi and/or melanoma. We will then examine the suspected area. The rest of the body will also be examined for moles.
If you have a suspicions growth, a biopsy will be taken. A small sample of tissue is removed from the area and sent for pathological examination. Anesthesia is injected under the skin to numb the area before the sample is taken.
Most biopsies for suspected skin cancers are done in the clinic. If the lesion is very small, all of it will be removed at the time of biopsy. If it does prove to be a basal cell or squamous cell cancer, but the outer edges are free of cancer cells, no further treatment is needed. If the outer edges do contain cancer cells, additional treatment is planned.
Larger and deeper biopsy samples are often needed to diagnose melanoma. Treatment will depend on the stage or extent of the disease.
Dr Touma has experience in the successful surgical treatments of over 5000 cases, most of them during his tenure at Boston University.
Treatment of skin cancer
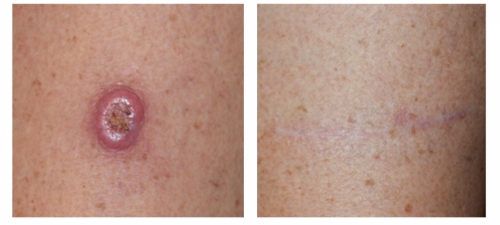
There are four main ways of treating skin cancer: excisional surgery (cutting the cancer out); electrodesiccation (destroying the cancer cells with heat); cryosurgery (freezing the cancer cells until they die); and radiation therapy in some cases, topical treatments with immunotherapy creams are successful.
The type of treatment chosen for basal cell or squamous cell cancer depends on how large the cancer is and where it is. If the sample taken for biopsy shows that cancer cells are present on the outer edges of the sample, we will go back into the area to remove any remaining cancer and a safety margin of cancer-free cells. For squamous cell cancers, which are more likely to spread, surgery may be followed by radiation or immunotherapy creams in some cases.
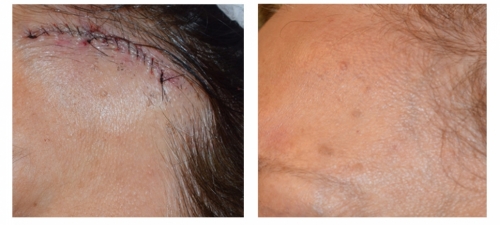
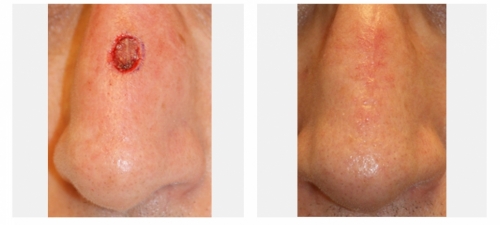
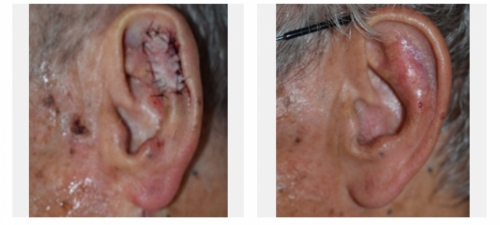
For cases that are in the delicate areas of the face such as those around the nose, lips, ear or around the eyes, or for cases that have recurred after prior treatment, especially among people younger than 60, the use of microscopically controlled surgery (Mohs surgery) is indicated. In this procedure, a thin slice of the cancer is removed and the bottom layer is examined for cancer cells. This process is repeated until a cancer-free layer is reached, and is associated with the highest possible cure rates.
Minimal normal tissue is removed in this procedure and the patient is spared the risk of a larger procedure. Also this technique leads to a better cosmetic result after surgery because of its tissue sparing effect leading to smaller scars. Mohs micrographic surgery is also done in some cases of skin cancer outside of the face, such as on the legs or arms, or whenever a smaller scar is desired. Mohs micrographic surgery is done in the clinic, under local anesthesia.

Dr. Touma has the largest experience in Mohs surgery in the Middle East, having treated over 5000 cases of skin cancer, and specializes in the cosmetic reconstruction of the skin after the precise removal of the skin cancer. In some cases, you may be referred to another physician for the reconstructive part of the procedure.
Surgery is the only way melanoma can be cured. Melanomas are usually larger and deeper than other forms of skin cancer and a larger safety margin is also removed.You may be referred to a surgical oncologist for a sentinel lymph mode biopsy, which will help determine the presence of cancer cells in the lymphatic drainage area. If the disease has already spread to nearby lymph nodes, these too will be removed. If melanoma has spread to more distant parts of the body, lymph nodes, skin, and underlying tissue there may also be removed. Although this cannot usually cure the cancer, in some cases, it could help relieve pain and lead to longer survival. Melanoma is best diagnosed early before it spreads outside of the skin, when it can be cured with surgical removal alone.
Chemotherapy treatment with anticancer drugs, has had only limited success in treating widespread melanoma. Because the standard methods of treating skin cancer have not been helpful for patients with later stage melanoma, these patients may be asked to consider experimental programs using new combinations of drugs and substances that can stimulate the body's immune system.

Follow-up care
Even when a skin cancer has been completely removed and is considered cured, follow-up examinations are needed to see if the cancer has returned, or recurred. That is most likely to happen in the first two years after treatment. In addition, a person who has had one skin cancer may still be at risk of developing another. Persons cured of skin cancer should continue to examine their skin every 6 to 8 weeks, have follow-up examinations as advised, and avoid overexposure to the sun. Dr Touma recommends exercise, smoking cessation, a sugar-free diet, and screening for other commn cancers, and family check-ups. In some cases, medications that decrease recurrence are prescribed.

Skin Graft
Expected survival times
Nearly 99% of basal cell and squamous cell cancers that are detected early and treated promptly are cured. For patients with melanoma and early stage disease, the chances of cure are greater if the cancer has not invaded deep into the skin. For patients with early-stage melanomas that are small, thin, and limited to a single area, the 5-year survival rate is about 91%. Once melanoma has spread to nearby areas, the survival rate falls.

Hope for the future
The real hope for the future lies in prevention and early detection of skin cancers. Most skin cancers can be prevented by avoiding overexposure to the sun. Any unusual growths or spots on the skin, especially any that change in size or color, should be checked by a dermatologist.
Scientists are now looking at ways of treating melanoma with substances that boost or reinforce the bodys own immune system. Of these substances melanoma vaccines and , interleukin-2 has had some success against melanoma. Ongoing studies will determine whether this treatment, perhaps combined with chemotherapy and other agents that act on the immune system(immunotherapy), will improve survival rates for patients with melanoma.

How to help guard against skin cancer
Don't get too much sun. Try to avoid the sun when its rays are strongest-between 10 a.m. and 3 p.m. Those who cannot avoid being exposed to the sun should wear clothing to cover up as much of the skin as possible. A sunscreen with a sun protection factor (SPF) of at least 15 should be applied to the exposed areas. Do not use sunlamps or go to tanning salons or parlors. Any usual blemish, mole, or other marking on the skin, especially one that changes in size or color, should be checked by a dermatologist.

View All Gallery




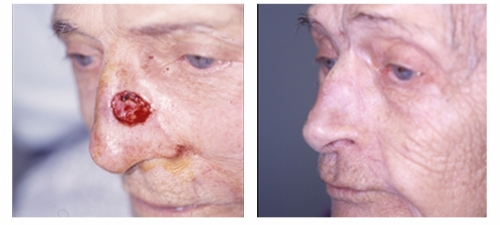


Dr Touma has the largest experience in treating skin cancer. His approach is highly customized to each case, and while he prefers Mohs surgery for most head and neck skin cancer in order to maximize cure rates and minimize scars, he has accumulated a large experience in treating skin cancer with topical immunomodulators or injection chemotherapy, laser or topical photodynamic therapy to achieve excellent cure rates and avoid scarring, and to try avoid unnecessary surgery or scarring from some of traditional destruction therapies such as cryotherapy.